Body Mechanics in Nursing⁚ A Comprehensive Guide
This comprehensive guide explores the crucial role of body mechanics in nursing practice. It details techniques for safe patient handling, injury prevention, and maintaining proper posture to optimize nurse well-being and patient care. Resources for further learning are also included.
Importance of Proper Body Mechanics for Nurses
Proper body mechanics are not merely a suggestion for nurses; they are a critical necessity for maintaining both physical well-being and the ability to deliver high-quality patient care. The physically demanding nature of nursing, involving frequent lifting, transferring, and repositioning of patients, places nurses at an elevated risk of developing musculoskeletal injuries (MSIs). These injuries can range from minor aches and pains to severe, career-ending conditions. Employing correct body mechanics significantly reduces this risk by distributing weight evenly, minimizing strain on the spine and joints, and promoting efficient movement. Beyond individual health, proper body mechanics is also crucial for patient safety. A nurse who is physically fit and injury-free can provide more effective and attentive care. By minimizing the risk of workplace injuries, healthcare facilities also benefit through reduced healthcare costs associated with worker’s compensation claims and improved staff retention rates. Ultimately, the implementation of proper body mechanics represents a holistic approach, benefiting both the nurses and the patients they serve.
Principles of Safe Patient Handling and Movement
Safe patient handling and movement hinge on a multifaceted approach prioritizing both patient and caregiver well-being. Prior to any movement, a thorough assessment of the patient’s physical capabilities, weight, and any pre-existing conditions is paramount. This assessment informs the choice of appropriate assistive devices, such as mechanical lifts or slide boards, and the selection of the most suitable transfer technique. Maintaining a wide, stable base of support is crucial, achieved by keeping feet shoulder-width apart. The body’s center of gravity should be kept low by bending at the knees and hips, minimizing strain on the back. Lifting should always be performed using leg muscles rather than back muscles, minimizing the risk of injury. When pushing or pulling objects, maintain a close proximity to minimize torque and leverage the body’s strength effectively. Smooth, controlled movements are preferred over jerky ones, reducing the potential for both patient and caregiver injury. Communication is key; clear instructions to the patient and collaborative teamwork during transfers are essential for a safe and successful outcome. Regular training and adherence to established protocols are crucial in ensuring consistent application of these principles.
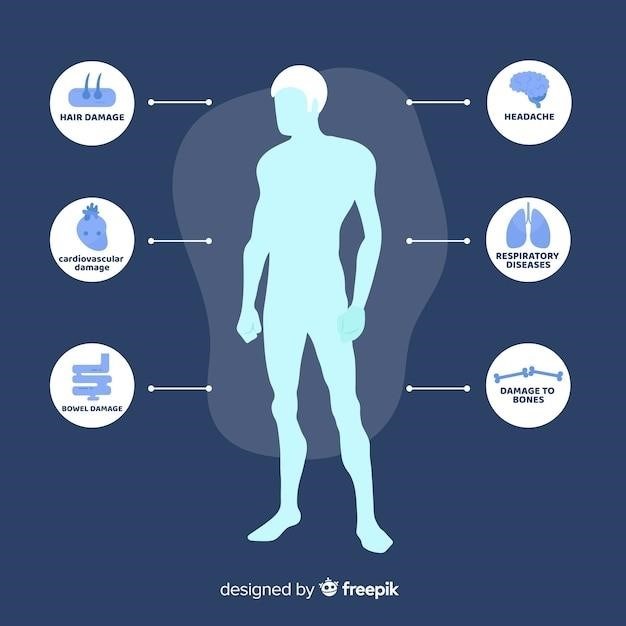
Preventing Musculoskeletal Injuries (MSIs) in Nursing
The physically demanding nature of nursing significantly elevates the risk of musculoskeletal injuries (MSIs). Proactive strategies are essential for mitigation. Prioritizing proper body mechanics during all tasks, from lifting patients to repositioning them in bed, is fundamental. This includes maintaining correct posture, utilizing leg strength for lifting, and avoiding twisting motions. Regular breaks throughout shifts allow for rest and recovery, preventing prolonged strain on muscles and joints. Staying hydrated throughout the day aids in maintaining muscle flexibility and reduces the risk of cramping. Adequate hydration is especially crucial during periods of intense physical activity. Utilizing assistive devices, such as patient lifts and slide boards, whenever feasible, significantly reduces the physical burden on nurses. Ergonomic assessments of the workplace identify and address potential hazards, such as improperly adjusted workstations or insufficient lighting. Furthermore, consistent participation in workplace safety training programs reinforces safe lifting techniques and promotes awareness of potential injury risks. Seeking early intervention for any developing musculoskeletal pain or discomfort is paramount; ignoring minor aches can lead to more significant problems later. A holistic approach integrating these preventative measures significantly reduces the incidence of MSIs in nursing.
Common Nursing Tasks and Proper Body Mechanics Techniques
Numerous nursing tasks demand meticulous attention to body mechanics. When transferring patients from bed to chair, maintaining a wide base of support, bending at the knees and hips, and keeping the back straight are crucial. Using assistive devices like gait belts enhances stability and reduces strain. During patient repositioning, employing proper techniques minimizes risk. For example, when turning a patient, the nurse should face the patient and use their legs to pivot, rather than twisting their back. When lifting objects, keeping the load close to the body, bending at the knees, and avoiding jerky movements is crucial. Pushing, rather than pulling, heavy objects conserves energy and reduces strain. Administering injections necessitates proper posture to maintain balance and avoid needle-stick injuries. While performing bed baths, maintaining good posture and utilizing support surfaces prevents fatigue and back strain. During wound care, adjusting the bed height and utilizing proper equipment facilitates efficient and safe wound management. Remember, consistent application of these principles minimizes the risk of injury across all nursing tasks. Each task should be evaluated for potential risks and a plan implemented to safeguard both the nurse and the patient.
Specific Body Mechanics for Lifting and Transferring Patients
Lifting and transferring patients require specialized body mechanics to ensure safety for both the patient and the caregiver. Before initiating any lift, assess the patient’s weight, mobility, and any potential pain or limitations. Always obtain assistance if needed, and utilize appropriate assistive devices such as slide boards, transfer belts, and mechanical lifts whenever possible. When lifting, maintain a wide base of support with feet shoulder-width apart. Bend at the hips and knees, keeping your back straight and engaging your leg muscles to perform the lift. Keep the load close to your body, minimizing leverage and strain on your back. Avoid twisting motions; instead, pivot your feet to change direction. When transferring a patient from bed to chair, use a smooth, controlled motion. Position the chair close to the bed and ensure the patient’s feet are firmly planted on the floor before assisting them to stand. If the patient requires significant assistance, employ a two-person lift technique with clear communication and coordinated movements. Remember to maintain proper body alignment throughout the transfer process to minimize the risk of injury. After the transfer, assess the patient for comfort and stability. Regularly review proper lifting techniques and incorporate them into daily practice to prevent musculoskeletal injuries.
Ergonomic Considerations in the Nursing Workplace
Creating an ergonomically sound nursing workplace is paramount for injury prevention. Assess the workspace for potential hazards, such as improperly adjusted furniture, awkward reaching, and repetitive movements. Ensure that beds, chairs, and work surfaces are at appropriate heights to minimize strain on the back, neck, and shoulders. Utilize adjustable chairs with good lumbar support to maintain proper posture during prolonged sitting. Promote the use of assistive devices, including mechanical lifts and slide boards, to reduce the need for manual lifting. Implement strategies to minimize repetitive tasks, such as utilizing automated systems for medication dispensing or charting. Encourage frequent breaks and position changes to avoid prolonged static postures. Provide staff with education on proper body mechanics and workplace ergonomics to foster a culture of safety. Regularly evaluate the workspace for ergonomic improvements and address any identified issues promptly. Advocate for ergonomic assessments and modifications to minimize the risk of musculoskeletal disorders among nurses. Collaboration between nurses, management, and occupational health professionals is crucial for creating a sustainable ergonomic environment. Remember that a well-designed workspace directly contributes to employee health and well-being.
Maintaining Proper Posture and Body Alignment
Maintaining proper posture and body alignment is fundamental to preventing musculoskeletal injuries. Begin by standing with feet shoulder-width apart, knees slightly bent, and maintaining a neutral spine. Avoid prolonged standing in one position; shift weight periodically to distribute pressure evenly. When lifting or transferring patients, keep your back straight, bend at the hips and knees, and engage your leg muscles. Avoid twisting or reaching; instead, pivot your feet to reposition yourself. When sitting, ensure your chair provides adequate lumbar support and allows for proper thigh and back alignment. Avoid slouching or hunching over. Take regular breaks to stretch and move around, improving circulation and reducing muscle fatigue. Be mindful of your posture when performing repetitive tasks, such as charting or medication administration. Regularly assess your posture throughout the day, making adjustments as needed. Consider using ergonomic accessories, such as back supports or wrist rests, to promote proper alignment. Proper posture and alignment not only prevent injuries but also enhance overall comfort and efficiency during work. Remember, maintaining optimal posture is an ongoing practice requiring conscious effort and attention to detail.
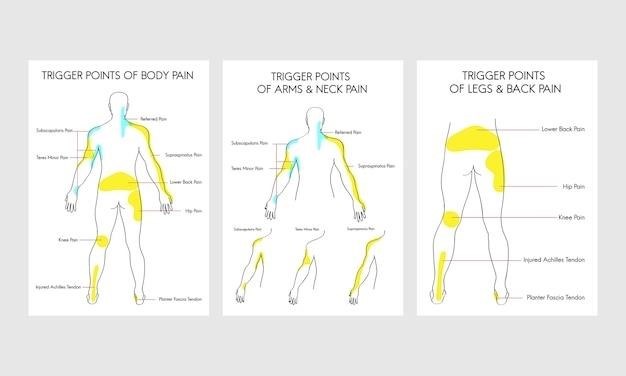
Addressing Back Pain and Other Musculoskeletal Issues
Back pain and other musculoskeletal issues are prevalent among nurses due to the physically demanding nature of the profession. Early recognition and intervention are crucial. If you experience back pain, consult with a healthcare professional for proper diagnosis and treatment. This may involve physical therapy, medication, or other interventions. Physical therapy can help strengthen core muscles, improve flexibility, and teach proper body mechanics. Medication may provide pain relief and reduce inflammation. Other interventions may include ergonomic assessments of your workplace and adjustments to your work routine. It is important to prioritize self-care and listen to your body. Avoid ignoring pain or pushing yourself beyond your limits. Take regular breaks, stretch, and use assistive devices when needed to reduce strain on your body. Maintaining good hydration and nutrition also supports overall musculoskeletal health. Employers play a vital role in providing a supportive environment, including ergonomic assessments, training on proper body mechanics, and access to healthcare professionals. By addressing back pain and other musculoskeletal issues promptly and proactively, nurses can maintain their physical well-being and continue their vital work.
Resources and Further Learning on Body Mechanics
Numerous resources are available for nurses seeking to enhance their understanding and application of body mechanics. Professional nursing organizations, such as the American Nurses Association (ANA), offer guidelines, educational materials, and continuing education courses focused on safe patient handling and movement. Many reputable online platforms provide comprehensive information on body mechanics, including videos demonstrating proper lifting techniques and interactive modules for self-paced learning. Textbooks and journals dedicated to nursing practice often include chapters or articles on body mechanics, offering in-depth explanations of principles and techniques. Workplace safety programs often incorporate training modules on body mechanics, tailored to the specific needs and tasks of healthcare settings. These programs may include hands-on training sessions with instructors who can provide personalized feedback and guidance. Furthermore, many universities and colleges offer specialized courses or workshops on ergonomics and body mechanics for healthcare professionals. These resources can help nurses stay updated on best practices and improve their skills in preventing musculoskeletal injuries. Remember to always consult with healthcare professionals for personalized advice and guidance on managing any musculoskeletal issues.